PEDIATRIC THERAPY REVENUE CYCLE MANAGEMENT
“Stop losing money to claim denials. Start maximizing your therapy reimbursements.”
Pediatric therapy practices face billing challenges that general medical billers
often do not understand. Authorization requirements for ongoing therapy sessions, specific
documentation needs for developmental conditions, and complex coding requirements can lead to costly
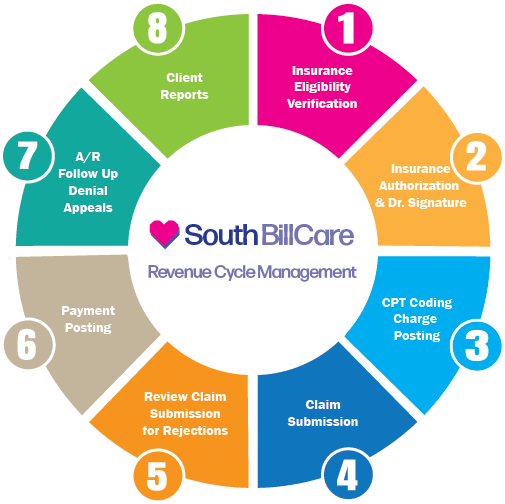
denials and delayed payments. At South Bill Care, we've built our entire revenue cycle management
system specifically for pediatric therapy practices because we know the difference between an OT
evaluation code and a PT progress note matters to your bottom line.
Our specialized pediatric RCM team has helped therapy practices increase efficiency up to 60% while
securing a 99% approval rate. Whether you're a speech therapy clinic struggling with Medicaid denials
or a multi-disciplinary practice facing insurance headaches, our exclusive focus on pediatric therapy
billing gives you an advantage that general medical billers can't match.
